February 13, 2026 | by Admin

For many women, period pain/menstrual cramps have been quietly accepted as part of life. Something to push through with hot water bottles and painkillers. Over time, this mindset makes it easy to ignore pain that disrupts work, sleep, and emotional well-being month after month.
Doctors at Petals Family Clinic, a woman and child care clinic in Kolkata, increasingly see patients who delayed seeking help because they believed suffering was normal.
The truth is simple but often overlooked: mild discomfort can be common, but intense or worsening cramps are not. When pain begins to control your routine, it may be a sign that your body is asking for attention.
Read on for deeper insights.
Painful cramps usually mean that the uterus is contracting more forcefully than it should, often due to underlying imbalances. When discomfort becomes intense enough to interfere with movement, focus, or sleep, it is rarely just sensitivity.
Several factors contribute, including excessive prostaglandins that intensify contractions, inflammatory responses, and internal changes. These affect how the uterus behaves during menstruation. Doctors look at patterns, not isolated cycles, to understand the root cause.
No—period pain is not normal when it regularly disrupts daily life or requires strong medication to function. While mild discomfort may come and go, severe menstrual cramps that stop routine activities signal something more than a typical cycle.

If pain feels stronger every month, lasts longer than expected, or forces cancellations, it may reflect deeper menstrual pain causes that deserve medical evaluation rather than endurance.
Cramping becomes concerning when it points to a medical condition rather than temporary discomfort. Pain that persists beyond menstruation or returns intensely each cycle is a common feature of chronic period pain.
Warning signs include severe cramps before menstruation- enough to affect sleep, pain spreading to the lower back or thighs, and symptoms gradually worsening with age rather than improving.
Not all period pain carries the same meaning, which is why recognising patterns matters.
| Feature | Typical Period Pain | Concerning Pain |
| Duration | 1–2 days | Several days or continuous |
| Relief | Improves with rest | Minimal relief |
| Activity impact | Mild discomfort | Daily tasks affected |
| Frequency | Occasional | Every cycle |
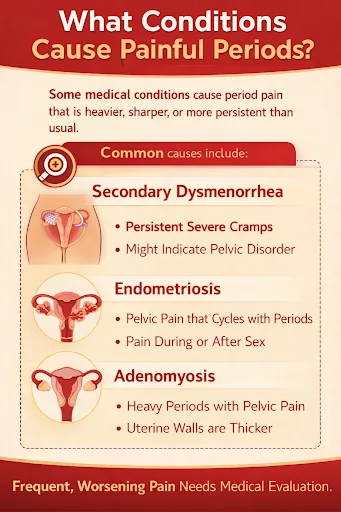
Certain medical conditions cause pain that feels heavier, sharper, or more persistent than usual. Doctors investigate these possibilities based on symptoms, age, and menstrual history. Common causes include secondary dysmenorrhea, endometriosis, and adenomyosis.
Hormones regulate how strongly the uterus contracts and how the body responds to inflammation. When this balance is disturbed, cramps intensify and linger, leading to hormonal imbalance and cramps.
At Petals Family Clinic, a woman and child care clinic in Kolkata, doctors recommend hormone testing to determine the underlying causes of menstrual pain.
Painful periods may also stem from metabolic or infectious conditions. PCOS and period pain often occur together due to irregular ovulation and ovarian cyst formation.
Infections are another contributor, especially when symptoms of Pelvic Inflammatory Disease, such as fever, unusual discharge, or pelvic tenderness, accompany cramps, increasing the risk of long-term complications if untreated.
Inflammation heightens the body’s sensitivity to pain signals during menstruation, especially when lifestyle stressors are present. Symptoms often include lower abdominal pain during periods, back pain during menstruation, and a sharper pain response even during normal uterine contractions.
Some menstrual symptoms must never be ignored, particularly when they appear together or worsen over time.
| Symptom | Why It Matters |
| Heavy periods with pain | May suggest adenomyosis or fibroids |
| Clotting during periods | Indicates abnormal uterine lining changes |
| Persistent cramps | May reflect structural or hormonal disorders |
| Pain during bowel movements | Often linked to endometriosis |
Pain becomes excessive when it interferes with normal functioning rather than remaining manageable. This includes pain that forces bed rest, repeated medication use, or emotional distress.
Doctors at Petals Family Clinic take symptoms seriously when pain scores remain high, nausea accompanies cramps, or discomfort persists outside the menstrual window.
Evaluation follows a structured approach rather than assumptions. Clinicians assess medical history, cycle patterns, and physical findings together.
Ultrasound imaging helps identify uterine fibroids, while blood tests rule out infection or endocrine imbalance. This method ensures accurate diagnosis without unnecessary treatment.
Delaying care allows symptoms to progress silently. Conditions like endometriosis often take 4-12 years to diagnose globally. (Source)
Early evaluation improves symptom control, preserves fertility, and reduces the emotional burden of recurring pain.
At our women and child care clinic in Kolkata, timely care leads to better long-term outcomes.
Menstrual pain should never be dismissed as a test of endurance. When cramps interfere with life, they reflect imbalance, inflammation, or disease rather than weakness. Early attention to your reproductive health protects it and helps you regain control over your body.
Schedule a consultation at Petals Family Clinic today.
Yes, stress can significantly worsen menstrual pain. Chronic stress increases cortisol levels, which can disrupt hormonal balance, trigger inflammation, and intensify uterine contractions, making period cramps feel stronger and more persistent.
Period pain may worsen with age due to hormonal changes, reduced physical activity, or the development of conditions like fibroids or endometriosis. Pain that intensifies over time should always be evaluated by a physician.
Yes, certain causes of painful periods, such as endometriosis or untreated pelvic infections, can impact fertility if left unmanaged. Early diagnosis and treatment greatly reduce long-term reproductive risks.
Ovulation pain can be linked to painful periods, especially in conditions involving ovarian cysts or hormonal imbalance. While mild discomfort is normal, recurring pain throughout the cycle requires medical attention.
No, home remedies may offer temporary relief, but do not treat the underlying cause. Persistent or recurring pain requires a proper medical diagnosis to prevent progression or complications.
Yes, lifestyle changes like regular exercise, stress management, balanced nutrition, and proper sleep can reduce inflammation and hormone imbalance, helping ease menstrual pain when combined with medical guidance.
Yes. Period pain can begin later due to hormonal changes, stress, weight fluctuations, or the development of conditions like fibroids or endometriosis.
Pain intensity varies depending on hormone levels, inflammation, stress, sleep quality, and lifestyle factors, all of which can influence uterine contractions.
Yes. Diets high in sugar and processed foods may increase inflammation, while a balanced diet can help reduce the severity of cramps over time.